“Perimenopause is not an illness. It’s a life stage.” - Gwen Floyd, CEO Wile
Perimenopause is what most people call “menopause.” It’s actually the first stage of menopause. And it’s driven by “sex” hormones, though stress and other hormones are players, too.
But if you’re experiencing this life phase, you’re not alone! 30M women are in perimenopause right now.
And understanding what to expect during this evolution can help you work with the changes, knowing up to 34 "symptoms" are totally normal. Knowledge, giving yourself grace and being aware of the different kinds of support are key.
Perimenopause Highlights:
- Perimenopause is what most people call “menopause.”
- It often lasts 2-3 years, but can last up to a decade.
- It typically begins in your mid-to-late 40s. But can start in the late 30s or early 50s.
- There are up to 34 different signs and symptoms.
- Most common signs: erratic periods, hot flashes/night sweats, interrupted sleep, mood swings, brain fog.
- No woman has exactly the same journey.
- It’s driven by the “sex” hormones but stress is a player and other hormones are, too.
Stages of Menopause
Menopause terms can be confusing. So before we talk about perimenopause, let’s look at the three stages of menopause:
-
Perimenopause
-
Menopause
-
Postmenopause
Perimenopause, meaning “around menopause,” is the transition period before menopause. Menopause itself is reached when we’ve gone a full 12 months without a menstruating.
And lastly, postmenopause immediately follows menopause. And postmenopause where we’ll remain for the rest of our lives.
Premenopause is actually the time between a woman’s first menstrual cycle and the beginning of perimenopause. In other words, premenopause is what we’ve been considering “normal” for the last while.
What is Perimenopause?
Perimenopause (or what most people call “menopause”) is also known as menopause transition, around menopause, or a late stage cycle. It’s when physiological changes (which occur in organ systems over time) happen before reaching menopause.
In our Western world, we often think of our bodies as separate parts and specific symptoms. But we’re one beautiful, connected system. So these physiological changes can include what’s happening in our brain, and our brain is impacted by the other systems in our body.
Mood changes are driven by transitions in body chemistry, including hormones. So if you feel or even think differently in this life stage, It’s not you, it’s your hormones (or at least, part of it is!).
Some say perimenopause is like reverse puberty. Like then, it’s a major shift in our bodies, minds and even self-identities. Yes, there can be hormone instability, mood swings, and WTH PMS symptoms along with a whole new period than you’re used to having.
Perimenopause can be intense—but also an incredible time of redefining who you want to be: independent along with a new self identity. So keep reading. Knowledge and awareness are power.
The Two Perimenopause Stages
Generally, perimenopause occurs in two stages: early menopausal transition (the early stage) and late menopausal transition (the late stage).
Early Stage Perimenopause
It can occur as early as your 30s, but typically happens in your early 40s.
Driven by hormone fluctuations, progesterone (the “chill out” steroid-hormone) decreases. And estrogen (the infamous “female” hormone) begins to fluctuate.
This causes a ripple effect of initial symptoms:
- Every-so-often skipped periods (consistent, 7+ day changes in cycle length)
- Hot flashes and night sweats
- Vaginal dryness
Late Stage Perimenopause
Most likely starts in your late 40s or early 50s.
And guess what? Even more hormone fluctuations happen: Progesterone further declines, while estrogen continues to fluctuate. Progesterone doesn’t balance estrogen like it used to, causing more bleeding during periods.
Add to the potential symptoms from earlier:
- Increased cycle irregularity
- Periods of skipped cycles of 60+ days
- Lasts for 1-3 years
- Continued PMS symptoms (those familiar sugar cravings!)
Eventually, your periods will stop. Then and only then will you know you’ve had your final menstrual period (FMP, because acronyms). Of course, if you’re not a data tracker, this may be hard to pinpoint or remember.
So female hormones like progesterone and estrogen are at play and fluctuating during perimenopause, causing a ripple effect on the rest of your body? They sure are. Here’s what’s going on behind the scenes.
Hormonal Changes in Perimenopause
In your 20s and 30s, hormones will typically be predictable. And when you’re in postmenopause, they’ll be consistent and low. But during perimenopause, your hormones will ebb and flow (and be less predictable).
As we get older, our egg population decreases and our ovaries create fewer “sex” hormones. But what are “sex” hormones, and what’s their role in all of these changes?
The "female" hormones are:
Estrogen - the poster child and most famous “female” hormone:- Is the one in charge of developing your reproductive organs and also the mother of the classic PMS symptoms, but supports too with cardiovascular health, cognitive function, and more
- Is also the “beauty” hormone - helping our bodies hold on to moisture, is part of hair regeneration and collagen production
- Affects metabolic function, and its decline during perimenopause can influence mid-body weight gain
- Is made by the ovaries, uterus and adrenal
- Beyond its abilities in the baby-making stages, it helps thwart heavy periods, calms mood and aids sleep
Testosterone - wait, what? Yes, this “male” hormone is part of our systems, and it helps with estrogen production, libido, and more
The Perimenopause Rollercoaster
Here’s where we start hanging on for the rollercoaster ride. Progesterone is the first to decrease (and somewhat steeply at that), then estrogen. However, this is not a steady decline. It ebbs and flows, which creates swings! Mood swings, sleep swings, period swings. You get the picture.
All while testosterone gradually declines.
What about the other hormones in perimenopause?
The shift in estrogen causes an increase in the Follicle Stimulating Hormone (FSH) and the Luteinising Hormone (LH), two hormones that team up to produce periods. Signal irregular menstruation and ovulation. And that’s only the beginning.
So when FSH levels go up and down, and ratios change, hang on for possible never-before-seen changes.
And here’s why these changes may feel even more new: For many years, the levels of estrogen, progesterone and testosterone likely ebbed and flowed in fairly consistent ways. Some of us are prone to heavy periods, PMS, period cravings - or whatever else.
When things drop below the norm, the ratios have changed. Estrogen may be far more dominant over generally lower progesterone (hello, PMS or heavy periods). As both decline, our testosterone levels are relatively higher than it’s been (What, me irritable?).
No surprise: you feel different, or you get a period, or pain or mood you’re unused to.

What are the First Signs of Perimenopause?
The “sex” hormones and other hormone changes trigger perimenopause likely (but not for-sure because we’re all different) symptoms. And here are some of the more common ones:
- Erratic cycles
- Hot flashes and night sweats
- Vaginal dryness
- Low mood
- Interrupted sleep
- Anxiety
- More cramping and worsening PMS
- Hormonal acne
- Interrupted sleep
- Changing moods
- Brain fog
But perimenopause looks different for everyone, so you might experience multiple symptoms early on, or hardly any at all. It’s not surprising then that when surveyed, half of the female respondents were in perimenopause and didn’t know or identify the signs. In some cases, they’d never even heard the word.
There are actually up to 34 perimenopause symptoms. Even before beginning perimenopause (premenopause), over half of women experience headaches, stiffness or aches in their joints, back pain, or difficulty concentrating.
How Long Does Perimenopause Last?
Perimenopause (from early-late) can continue up to a decade. But on average, perimenopause lasts 2-3 years.
- Around 35 or 40, our female hormone levels naturally start to decrease
- After age 40, we experience continued hormone fluctuations
- Age 46-53, perimenopause typically makes its grand entrance into our lives
- But (of course, there’s a but), we can notice symptoms as early as our 30s
But like we said earlier, everyone’s transition looks different. Some experience changes for as little as a few months or for as long as a decade or more.
Keep in mind too that it's possible to be fertile during perimenopause, and you can become pregnant. Continuing to have birth control options is important!
What's the Best Supplement for Women Suffering from Perimenopause?
We’re a supplement company, so we had to get here eventually, right?
And full disclosure: Google let us know that “Suffering” was the word most women search for.
Let’s try and do something about that!
You can ask your doctor. But….
Most traditional M.D.s, including OB/GYNs, have very limited education in both nutrition and in menopause. Check out our latest blog: 'Read This Before Your Next OB'GYN Appointment'.
According to the journal Academic Medicine, only 27% of U.S. medical schools gave med students the 25 hours of recommended nutritional education.
And even that would only clock in 6.25 hours of training per year.
And then, there’s the OB/GYNs. The most recent (and small) survey of OB/GYN residents showed fewer than 20% received formal training in perimenopause or menopausal care.
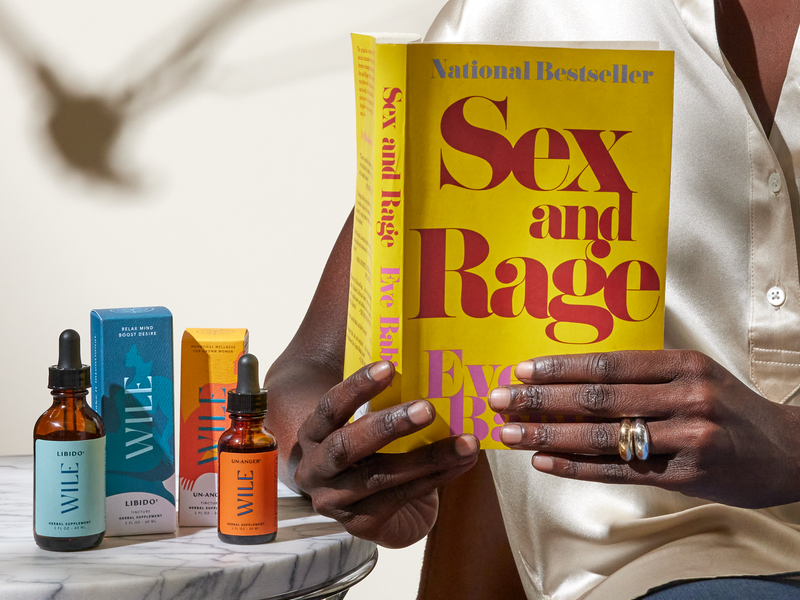
Wile’s Approach to Perimenopausal Supplements: Not One Pill Fits All
There is no single “best” supplement for any one woman - and that’s exactly why we formulated Wile the way we did.
Our hormones are complex and ever-changing, signaling a myriad of calls and responses in the body and mind. Read more on this in our 'Hormones & Crosstalk' blog. That’s where the 34 perimenopausal symptoms or signs come in.
Wile perimenopausal line is a series of daily capsules that can work together or separately to meet your needs, from pre-peri through menopause (with some benefits even after, but that’s another subject).
The best supplements for perimenopause include natural phytoestrogens, estrogen-mimicking compounds naturally occurring in plants, rather than synthetic hormones. Estrogen levels are critical to emotional and hormonal well-being, and that’s why our go-to is our Perimenopause Support supplement.
Here’s how it works:

Works across the whole system affected by these hormonal shifts, to help bring about more regulation overall. It also helps boost the results of the rest of our products.
- Endocrine (sex hormones) - phytoestrogens
- Adrenals (stress centers, all kind of cortisol) - adaptogens for stress
- Nervous system (to soothe the nervous system) -nervines to help regulate the nervous system
- Nutritives that help the body use all that good stuff
From there, mix and match according to your specific needs.
The Journal of Neuroinflammation states around 1.3 million women reach menopause every year. And the transition before menopause includes hormonal changes that can affect us in many different ways.
But at Wile, we want to make perimenopause a journey we talk about, learn about and use to help us get to know ourselves in new ways. And we are here to help you make the next phase yours. It’s your power; take it!
This article is intended for informational purposes and is not intended to replace a one-on-one medical consultation with a professional. Wile, Inc researches and shares information and advice from our own research and advisors. We encourage every woman to research, ask questions and speak to a trusted health care professional to make her own best decisions.