It's the day we love to hate. Or maybe just… hate to hate. It’s the annual OB/GYN visit. Spoiler alert: they have yet to design a better speculum.
You’d be surprised to know that there are many things that your OB/GYN may need to upgrade in terms of knowledge—things that you might be experiencing every day. In this post, we’re going to talk about things your OB/GYN might not know and some tips for being your own health advocate.
OB/GYN is Now a Female-Dominated Profession
Gynecology dates back to Greco-Roman civilization, if not earlier—and since then, it was a male-dominated field… until very recently. A 2019 study revealed that 82.85% of OB/GYN practitioners in the United States were female. In the olden, male-dominated days of obstetrics and gynecology, women faced challenges that we are lucky to be largely spared today: flawed logic about the human body, crazy theories about cures, and techniques developed without the consent of female patients were the norm.
Now, an overwhelming number of students in the OB/GYN stream are women. We live in a modern world where male gynecologists will often bring a female colleague into the room with them during examinations out of consideration to ensure the patient is more comfortable and there are no miscommunications.
This change has been largely beneficial when it comes to women's care, but it has had one drawback: fewer individuals qualifying as OB/GYNs have led to a shortage of female health practitioners around the country.
Medical Gaslighting: Doctors Are More Likely to Dismiss Women’s Pain
Countless women have shared their stories of reporting serious pain to their OB/GYNs, only to be dismissed, misdiagnosed, or pacified. This is a problem for all women, but medical gaslighting is a particularly large problem amongst Black women and NBWOC.
Some of the shocking findings over the years have shown that:
- Women are typically prescribed less pain medication than men after undergoing the same procedures.
- Women are less likely to be admitted to the hospital or receive stress tests when experiencing chest pain.
This is similar to what many women suffering from gynecological issues like endometriosis or PCOS face when trying to seek treatment for pain and heavy bleeding from their GP or OB/GYN. The time to diagnose endometriosis is four to eleven years after first experiencing symptoms. This is largely due to misbelief and minimization of patient pain on the side of the health practitioner.
Early detection can be a differentiator, but because so many women are dismissed by their doctors when reporting their symptoms, it's often only detected when treatment becomes more difficult and expensive. For women from lower-income backgrounds, this can be especially detrimental. When a woman has had a negative experience with a medical professional, especially about a deeply personal thing like their body, they are less likely to get the treatment they need. In the cases of serious illnesses where early prevention is key, this can be a staggering blow.
Self-Advocacy Isn’t Easy
One of the most recent public examples of medical gaslighting happened to tennis star Serena Williams. Speaking to Vogue in 2018, Williams discussed an incident in which a nurse and medical team did not listen to her fears of pulmonary embolism following the birth of her daughter, Olympia. When they finally gave in and ran a CAT scan, Williams was found to have several small clots in her lungs.
While this type of patient treatment isn’t always intentional, it’s an example of unconscious bias in the medical field that causes endless harm to women. As a woman, the quickest way to get the care you need is to become a fierce ally for yourself and your body. You know your body better than anyone else. If something is wrong, keep going until you find a medical professional that is willing to listen. If you’re one of the countless women who have been told to suck it up or that it’s “not that bad,” don’t give up until you find a doctor who listens to you and your concerns. Never be afraid to seek a second—or third, or fourth—opinion until you’re confident that you have been heard and treated with the proper amount of care and attention.
There are OB/GYNs out there who know that they might not always know. Find the doctors that are willing to play ball when it comes to discussing your individual needs and experiences. Know your rights and always trust your instincts.
Let’s Talk About The Pill
Many gynecologists use hormonal contraceptives like a cure-all: Painful periods? Birth control. Bad skin? Birth control. Mood swings? Birth control. And while contraception has come a long way in the past few decades, there isn’t enough information about the long-term effects it can have on your body and mental health for it to be the go-to solution that so many healthcare providers treat it as. Contraception options like the pill are sometimes used to treat the worst of the symptoms associated with pain and bleeding, but there are also caveats to be aware of that have been under-reported in the past.
New research has indicated that the risks of taking birth control for prolonged periods of time might be higher than initially expected by doctors, although many health practitioners remain unaware of the consequences.
For many women, long-term use of hormonal contraception can cause:
- Higher blood pressure
- Increased risk of blood clots
- Hypertension
- Increased risk of cervical cancer
- Other medical issues
These adverse risks should also be considered when talking about Hormone Replacement Therapy—but know that the typical estrogen loads in those treatments are often a fraction of what you’d get in the pill.
There’s Not Enough Research About Women’s Reproductive Health
Something that you and your gynecologist might not know is exactly how limited studies into female reproductive health even are.
Since a health issue like endometriosis only affects a portion of the population, it’s less appealing to scientists than an all-encompassing issue like diabetes or cancer which affects all genders. Does it mean endometriosis or PCOS is less serious? Absolutely not. Does it suck? Oh, hell yes. The lack of scientific research means that there have been few treatment breakthroughs in the past few years. It also means that we don’t know the root cause, or how to develop a potential cure.
Another challenge when it comes to studying women’s reproductive health is that symptoms can vary so much between individuals and might present differently from what is described in medical journals. This means that despite their best intentions, a doctor might not immediately make the correct diagnosis.
The problems with research into female health extend to covering the experiences of people of color and the LGBTQ+ community. These are communities that are typically already underserved when it comes to healthcare, and discrimination within the medical communities means that they are even further isolated from receiving proper care or taking steps to see a professional for a medical issue.
There is some hope, however. These days, female physicians of all specialties (particularly gynecology) are more likely to be nonwhite women. This is changing how many gynecological patients experience their primary healthcare and indicates that we are—slowly but surely— moving towards a future where everyone’s voices are heard. It’s also increasing the services available to previously underserved communities.
Patients Talk Differently To Female OB/GYNs Than Male Ones
Recent research findings have indicated that when it comes to gynecology, patients are more inclined to reveal more medical information to female doctors than they would their male counterparts. This includes making more affirmative statements and being more assertive when discussing their medical issues.
Why is this? First of all, speaking about your issues woman-to-woman feels more natural—female gynecologists can typically make recommendations out of their personal experience as well as their professional knowledge. When it comes to that embarrassing lump, it sometimes just feels easier to get into the nitty-gritty with a lady doctor.
Another reason is that many women find the idea of discussing intimate medical issues with men intimidating. This isn’t always due to the actions of the male health practitioner himself, but more due to growing up with the social stigma that anything related to your vagina can not be discussed in the presence of men. In some cultures, seeing a male doctor for your personal health is frowned upon. For some women, having a male gynecologist doesn't matter at all. For others, it's a fear that can reduce their likelihood to seek care in the future.
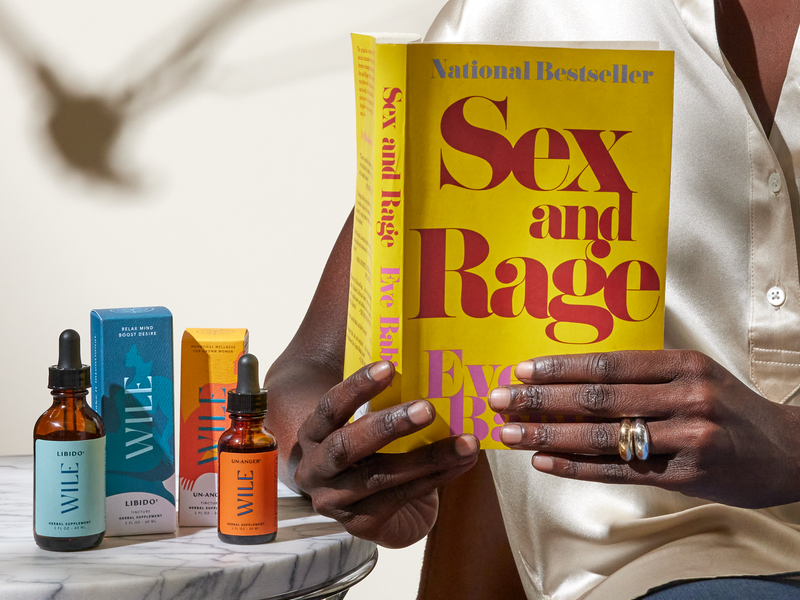
Wile’s In Your Corner
At Wile, we understand what it’s like to be a middle-aged woman—we’re all there ourselves. We aim to empower aging women with knowledge, know-how, and supplements to help in this chapter of life.
Wile’s supplements contain hard-working plant ingredients to help ease symptoms of burnout, stress, menopause, and more. Wile’s products allow you to feel like you again without synthetic formulas. We use clinically backed adaptogens and phytoestrogens nervines to help support an aging woman’s unique needs.
This article is intended for informational purposes and is not intended to replace a one-on-one medical consultation with a professional. Wile, Inc researches and shares information and advice from our own research and advisors. We encourage every woman to research, ask questions and speak to a trusted health care professional to make her own best decisions.