The internet is awash in all things “period” these days. Books, kits, and even parties are devoted to our first entry into the menstruation station. Yet there’s little information on what to expect from your period after 40. Ovulation, period cups, and egg freezing have all gotten glow-ups, yet what happens once hormones start to downshift is still out of the conversation.
Why? There’s been an ageist association—and with it, fear—that comes from even uttering the word “menopause.”
It’s not surprising that when surveyed, half of the female respondents were in the perimenopause stage and did not know or identify the signs. In some cases, they’d never even heard the word.
Just like you, your period is something that will change over time and not always predictably. It’s our goal to make sure you are familiar with potential changes and how to best prepare for them.
Welcome to your period after 40; a slightly unpredictable rollercoaster, but one that ultimately comes to an end. This is what to know about how your period can change.
Know That Anything Can Happen (And Not Happen)
This is an introduction to the common milestones on the journey of your period after 40, but truly everything and nothing is “normal.” We have friends who have experienced extreme periods and others that had theirs simply taper off and go away with little drama. Some had hot flashes for 10 years and others had none whatsoever.
The fascinating and infuriating part is that every single person experiences this differently. What happened for your mom, aunt or biological sister is not necessarily going to happen for you.
And there is no way to know for sure when or how it will affect you until it does. What we do know is that getting ahead of these changes and smoothing out the balance can be remarkably beneficial and the earlier, the better.
For most of us, we are our own first warning sign—no one knows your body better than you, so if something is feeling different, pay attention.
We’re focusing on the most common “period-related” signs of changes here, but there are many more signs or “symptoms” of perimenopause.
Phases Of The Menstrual Cycle And How They Change
Basics first. If you remember your sex ed days, the menstrual cycle is divided into four main phases:
- The menstruation phase is the shedding of the thickened lining of the uterus.
- The follicular phase can be thought of as the body’s hormones preparing an egg for potential fertilization or pregnancy.
- Ovulation.
- The luteal phase ensures the right hormones are released to create an ideal space for the egg to be fertilized.
Black and brown women often experience these changes a little earlier and often with more intensity than white or Asian women. Why? No one is entirely sure because the medical community has not seen it fit to devote as many resources to this life stage in general, let alone understanding its impacts on women of color. As a result, studies in this area have been limited.
We do know that because estrogen and progesterone levels are changing in your body during this phase, it’s likely they will not be working in the same balance as they did for many menstruating years, We’re calling that the “before” period.
It’s important to bear in mind that while you are perimenopausal - meaning even when your period is not monthly or regular - you could still be fertile and can become pregnant. Having birth control options available during this stage of your life remains important.
This happens as your body produces fewer hormones during the follicular and luteal phases until you stop ovulating altogether and reach the final menopause stage.
Call it perimenopause, pre-menopause, or just a late-stage cycle, these are all signs that things are changing in your body, and like when you were a teen, it might not always feel that great.
The First Sign? Often More Cramping, PMS, And The Possible Return Of Hormonal Acne
Some women report feeling more “moody” during their period or have noticeably worse PMS than they experienced throughout their 20s and 30s. Often it can feel like a return to your teen years. And it kind of is, with breakouts and I-hate-the-world vibe that can come with it. Some women’s health practitioners describe this phase of life as “puberty in reverse”.
This PMS effect is thanks to estrogen, the mother of the classic PMS symptoms - cravings, edginess, impatience, headaches, cramps. In your “before” period, estrogen was balanced by a big surge of progesterone occurring when an egg is released.
You may have less progesterone to surge or the occasional cycle with no egg to release (called anovulatory cycle).
Yet your ovaries are cranking out the estrogen to release an egg. Without the surge of progesterone, there’s no chill vibe to balance out the big E. This estrogen dominance = more PMS.
Our Perimenopause Support supplement can help this balance at any stage - before you begin to see symptoms, after they’ve shown up or even well into menopause. Taken early and daily, it evens out the period after 40 problems that start before we even think “perimenopause” and long after.
Expect: Weird, “WTH Is This?” Periods
When you’re having your period after 40, you may already have noticed less regular periods vs what has been “normal” for you in the past.
From your late-30s to your mid-40s, you may find the length and flow of your normal period subtly (or dramatically) changing. This early introduction to signs, aka menopause ‘symptoms’ can last up to four years on average, although some experience them only for a few months.
As your usual hormonal levels start to shift and change, you may notice some of the following changes in your period after 40:
- Lighter bleeding then in the past.
- Longer and/or less defined periods for your periods.
- Heavier bleeding and cramping then in the past. You may be reaching for a super plus tampon for the first time in your life. Yes, that’s “normal’ and a sign of shifting hormones.
- Sparse spotting or skipping periods altogether.
Again, a changing balance of progesterone and estrogen is at play. More estrogen and/or relatively less progesterone can lead to heavier or less predictable bleeding as progesterone mellows the effects of estrogen on your uterine lining and shedding, not just your mood.
Then as estrogen declines, there is less flow.
These declines are normal, of course. But the imbalance between the two is what can cause the disruptive periods.
Chronic stress only exacerbates this, as ongoing stress lowers the body’s production of progesterone on top of its regularly scheduled changes.
Expect: Bloating
Hormonal changes can create havoc with the way our bodies retain moisture. Often we may experience bloat just as we usually experience with our periods, and also see swelling around the ankles, wrists, and other major joints as is common in pregnancy when hormones shift. Increased water retention is something that many women report happening when keeping track of their period symptoms after 40.
Expect: Breast Tenderness
Again, as often happens early in our period days and in pregnancy, the hormonal shifts can bring about bodily issues like breast tenderness, soreness, and even burning. Yes, burning.
This type of niggling pain can be particularly annoying, and while it will likely resolve itself over time, there are a few things that you can do to take the edge off (and no, we don’t mean having that extra glass of wine!).
For breast tenderness associated with your period, try:
- Ensuring you’re wearing a comfortable but supportive bra.
- Using warm or cold compresses.
- Cutting down on caffeine.
- Please eliminate other potential causes by speaking to your doctor or health practitioner.
Is It My Period? Or Is It Perimenopause?
The majority of women go through a menopausal transition between the ages of 45 and 50. 47 seems to be the “magic” age when perimenopausal changes often start to be more pronounced, with 51 being the common point for “menopause” to hit.
Menopause is actually defined as the day you’ve gone 12 full months without a period. There are plenty of other changes that may happen between the first sign of a more intense PMS or a slightly unusual period.
Perimenopause Is NOT A Disease
A changing period is scary, especially if yours has been quite regular for most of your life.
We’re wired to have the first warning bells say, “I’m pregnant?!?!”
The second is often: “Oh no, is something wrong with me?”
And the third? Menopause. Which can be the scariest of all.
Younger women have pushed against body image and slut-shaming, it’s up to Gen X and Xennials to reject these dated and inherently misogynist stigmas against our periods and bodies changing. We will decide who we are and how we feel about these changes and the bodies we get to live in, often for another half of our lives.
So try to put aside any negative thoughts that you might have previously associated with this process. We want to make perimenopause and menopause something we learn about, talk about and use as a way to get to know ourselves in new ways.
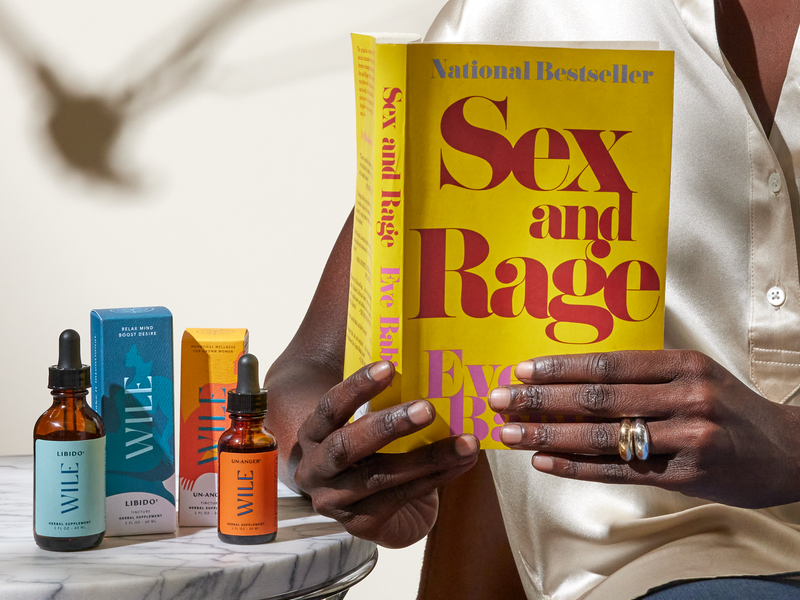
At Wile, we’re here to help. Our Perimenopause Support blend is made to make these transitions easier. It provides a strong baseline for overall hormonal wellness that can be customized with other Wile formulas to meet your moment.
Our 40+ Period Support supplement is specifically for the changing cycles that cn start even in your late 30s. It helps ease painful periods and cramps, the resurgence of serious PMS, or to manage erratic or heavy bleeding that starts after 40. You don't need synthetic hormones for an easier cycle in this changing phase.
Why deny, fear or shame the changes in your body when you can work with them? Make the next phase yours by owning the incredible power of your hormones and of plant allies.
Photo credit: Jovis Aloor via Unsplash
This article is intended for informational purposes and is not intended to replace a one-on-one medical consultation with a professional. Wile, Inc researches and shares information and advice from our own research and advisors. We encourage every woman to research, ask questions and speak to a trusted health care professional to make her own best decisions.