We hear it all the time.
A woman is over 40 (or over 45) and seeing changes in her period, cramps, hot flashes, sleep, maybe mood.
Often we go to our doctor for advice on perimenopausal symptoms and the only medical advice is,, “Go on the Pill.”
The other advice is often, “You’ll just have to stick it out, which arguably is worse, but we digress.
Many women will choose to go on the Pill for perimenopausal symptoms. Or perhaps or stay on the Pill for perimenopausal symptoms.
If that works for you, great. However, there are other options, even if your doctor is not well versed in them. Here are things to consider if your doctor recommends the Pill for perimenopause.
1. The Pill was not designed as a perimenopause treatment.
Prescription medications get relabelled for other ailments all the time (Botox™ injections started as treatments for headaches and sweating, after all). The thing is, the hormone levels in the Pill are designed very specifically to block contraception in fertile women. Many of us were put on the Pill as teens, ostensibly to reduce heavy cramps, bleeding or PMS. So if that was you 25 or 30 years ago, this idea may seem to make sense.
However, the hormone levels in birth control were not designed to deal with the constantly fluctuating hormone levels of a woman over 40 (or 45). Read on for why that could be complicated.
2. The hormone levels in the pill could push estrogen dominance.
The levels of hormones in the Pill can create an overabundance of estrogen in the body. This is not necessary and sometimes is linked to a host of other possible health concerns.
3. Perimenopausal hormones (even before you know it's perimenopause) are in flux.
Typically, progesterone drops first, then estrogen, with fluctuations in between. This is very different from the way your hormones were produced in your most fertile years. The Pill’s levels may react very differently with your body than they did a few years ago when you were in peak fertility.
4. The Pill could make perimenopausal symptoms worse.
Friend of Wile and integrative nutritionist, former nurse and menopause expert Esther Blum, says it best: “Birth control pills suppress the body's own progesterone and ovulation. As we move towards and through menopause, progesterone levels naturally fall on their own. So chemical contraception only fuels the hormonal fire of rock bottom progesterone, which can lead to:
Insomnia
Worry
Estrogen dominance
Hot flashes
Night sweats
Weight gain
Brain fog
Fluid retention
…And more.”
Progesterin-only mini-pills have their own potential complications as again, they are dosed for fertile women to suppress pregnancy. It is not progesterone planned for the falling (and fluxing) levels once perimenopause begins.
Note: Typically, the Pill uses progestin, which is similar to but not the same as the body's progesterone. HRT typically recommends progesterone vs progestins.
5. Many of us didn’t do well on the Pill in the first place.
Often we were already off the Pill for a reason. Many of us had unwanted side effects when it was used for necessary contraception. It’s just not as simple as the general mindset wants it to be.
6. What if you can’t go on the Pill?
A history of blood clots or other issues may have kept you off the pill anyway. This means the simple go-to will not be an option. Your health care provider should be more informed, accepting and proactive about other options, be they topical estrogen, progesterone, nutritional changes and natural remedies. But often, that’s not the case.
Since only a fraction of OB/GYNs felt they got adequate training on menopause, it can be hard to find a well-rounded source of guidance.
7. The pill can complicate your vascular system and metabolism (both of which can be concerns in perimenopause and post-menopause).
Wile’s naturopathic physician advisor, Dr. Jillian Stansbury pointed out the other issues. “The pill puts a big hormone burden on the liver and can contribute to blood clots and vascular inflammation,” Dr. Stansbury said. Hot flashes and night sweats are actually vasomotor (vascular) events.
8. You’ll probably get your period even longer.
The hormones in birth control pills may keep your period going far longer or otherwise disrupt it. Indeed, some medical advice says the only way to know if you’re truly menopausal is to go off the Pill for a few months. Does anyone else find that a bit head-scratching? Will you then simply be on the Pill indefinitely? And what might that mean for your overall health?
9. Your doctor may not be an expert in perimenopause - even if they’re an OB/GYN.
The Mayo Clinic reported a survey in which residents in family medicine, internal medicine and obstetrics-gynecology in 20 programs were surveyed on their preparation to serve perimenopausal and post-menopausal women. Of the respondents:
- 20% reported getting no menopause lectures as part of their residency
- Less than 7% said they felt “adequately prepared to manage women experiencing menopause”*
*sort of an odd way to phrase it, if you ask us.
While it should always be a woman’s choice on how to guide her health, we encourage women to investigate:
- HRT which is designed more appropriately to alleviate issues specifically related to perimenopause in a safe and effective manner.
- Non-ingested estrogen replacements, especially if taking estrogen is not a good option for you
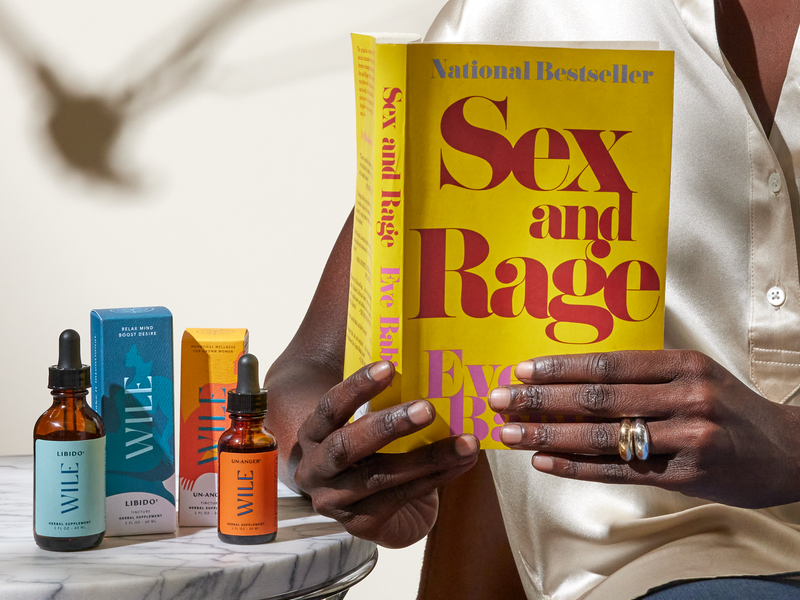
- Natural remedies like Wile, based on the natural approaches of Eastern medicine, naturopathy and other holistic modalities which, unlike Western medicine, have been treating, researching and working with perimenopause for centuries.
All of our Wile capsules are designed to mix and match to meet your particular journey, from early days when hormones first shift through menopause and even beyond.
Perimenopause Support – get better overall balance in sleep, PMS, mood, hot flashes and focus.
40+ Period Support – helps ease painful, erratic, heavy periods and intensified PMS (from first signs of period changes through perimenopause)
Hot Flash – manage hot flashes and night sweats
Women's Stress –increased stress resilience, focus and overall well-being, with fewer mood swings caused by 40+ hormonal shifts and/or life.
By taking what you need and nothing you don’t, your body is in a better balance and you know where you’re at. Take what you need, nothing you don’t and adjust as your body does (because it’s very likely you will keep changing). Our product quiz is a great place to start.
- Other integrative practices such as Traditional Chinese Medicine and acupuncture, diet and lifestyle changes to make this transition a positive and powerful one.
ADDITIONAL SOURCES:
Kling, Juliana M. (MD) et al, Menopause Management Knowledge in Postgraduate Family Medicine, Internal Medicine, and Obstetrics and Gynecology Residents: A Cross-Sectional Survey, Feb 1 2019This article is intended for informational purposes and is not intended to replace a one-on-one medical consultation with a professional. Wile, Inc researches and shares information and advice from our own research and advisors. We encourage every woman to research, ask questions and speak to a trusted health care professional to make her own best decisions.